In recent years, Photobiomodulation (PBM) therapy has been gaining widespread attention from the global medical community as a non-drug treatment option for Parkinson’s Disease (PD).
According to several clinical studies published in 2023, PBM therapy using specific wavelengths of red and near-infrared (NIR) light has shown effectiveness in alleviating symptoms of Parkinson’s, improving motor function, and enhancing quality of life.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10819946/
- https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-024-03857-z
- and over 10 other studies
More specifically, PBM therapy has been shown to activate mitochondrial function in the brain, promoting the survival and regeneration of neurons while suppressing inflammatory responses, thereby delivering neuroprotective effects.
These studies indicate that PBM therapy may complement or potentially replace traditional drug treatments and merit serious attention for their implications in Parkinson’s care.
The Realistic Limitations of Modern Parkinson’s Treatment and Drug Side Effects

Parkinson’s Disease is still considered incurable and is typically treated with dopamine-replacement medications. However, long-term use of these medications inevitably leads to reduced effectiveness and may cause serious side effects such as dyskinesia, hallucinations, and cognitive decline.
As a result, patients often experience a gradual decline in quality of life and worsening symptoms, falling into a vicious cycle. Due to these limitations, there is a growing need for safer, long-term, non-invasive treatment methods with minimal side effects, which further underscores the value of PBM therapy.
Parkinson’s: Not Just a Brain Disorder, But a Systemic Condition
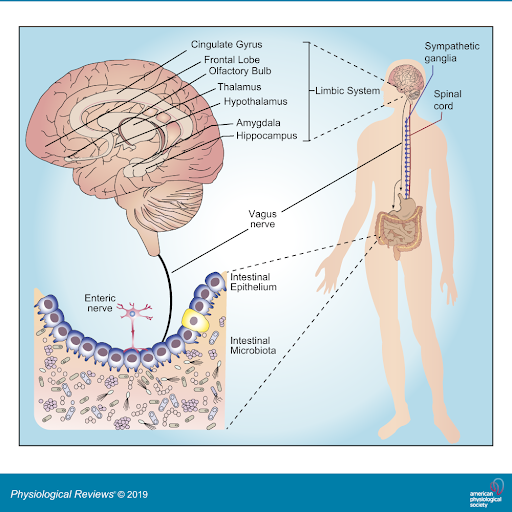
Recent research shows that Parkinson’s is not limited to issues in dopamine-producing brain cells. it is closely related to various physiological changes throughout the entire body. CN X Vagus nerve connects the organs to the brain. Therefore, changing the atmosphere of the gut microbes may have an impact on the brain
In particular, many studies have suggested that abnormal accumulation of alpha-synuclein and gut microbiota imbalance are key pathological factors in Parkinson’s Disease. Alpha-synuclein is formed not only in the brain but also in the gut. Imbalanced gut microbiota (dysbiosis) may promote the pathological spread of alpha-synuclein, which can reach the brain—this forms the basis of the “gut-brain axis” hypothesis.
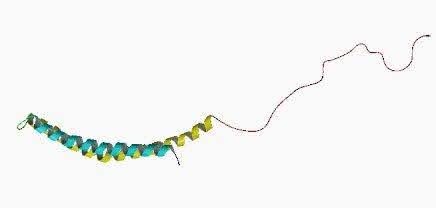
Molecular structure of α-synuclein: The helical structure of the N-terminal domain (green) is most characteristic. This new theoretical perspective suggests that Parkinson’s Disease should be treated as a systemic condition, not just a localized brain disorder.
Why Parkinson’s Treatment Should Shift from Localized to Systemic
The gut-brain axis hypothesis makes it clear that Parkinson’s treatment must evolve beyond simply supplementing dopamine in the brain—it requires a whole-body therapeutic approach.
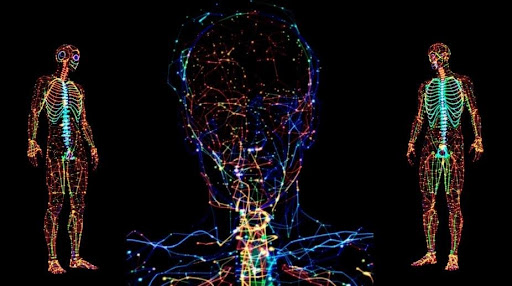
PBM therapy involves the delivery of red and near-infrared light through the skin, penetrating deeply into the body to activate mitochondrial function, reduce systemic inflammation, and help regulate gut microbiota balance.
This systemic therapeutic mechanism may positively influence not only the nervous system, but also the digestive system, hormonal balance, and the immune system—offering a pathway to address the root causes of Parkinson’s Disease.
Thus, this suggests the need for systemic PBM therapy rather than localized treatment.
Clinical Trials and Progress in Systemic PBM Therapy for Parkinson’s
Clinical trials using PBM devices are actively ongoing worldwide. In South Korea, Pusan National University Yangsan Hospital is currently conducting clinical research on PBM therapy for Parkinson’s patients.
This study applies specific wavelengths of red and NIR light optimized for Parkinson’s treatment using full-body PBM equipment. Key indicators being evaluated include improvements in motor function, cognitive function, and quality of life.

Early clinical results suggest that systemic PBM therapy can significantly improve both motor and non-motor symptoms, along with overall quality of life.
These PBM devices allow patients to comfortably lie down while receiving 20-minute full-body light treatment. They cause little to no discomfort during treatment and have virtually no side effects.
Since the devices must deliver optimal light to the body, they are intricately designed with complex parameters such as light wavelength, power pulses, spatial configuration, and internal materials.
With more studies in the pipeline, systemic PBM therapy holds promise for commercialization and standardization in Parkinson’s care—potentially marking a paradigm shift in treatment strategies.
Related Article: Natural Treatments for Parkinson’s Disease
Conclusion: From Localized PBM to Comprehensive, Whole-Body Strategy
While previous studies on localized PBM therapy confirmed some potential, they have been insufficient in addressing the complex pathophysiology of Parkinson’s Disease.
Now, we are moving toward a more holistic, whole-body therapeutic strategy.
This evolving approach is expected to greatly contribute to improving the quality of life and expanding treatment possibilities for patients with Parkinson’s Disease.













