A middle school student taking diabetes medication?
In 2025 Korea, middle schoolers are taking diabetes medication, high school students are on blood-pressure medication, and even elementary school children are being diagnosed with fatty liver disease.
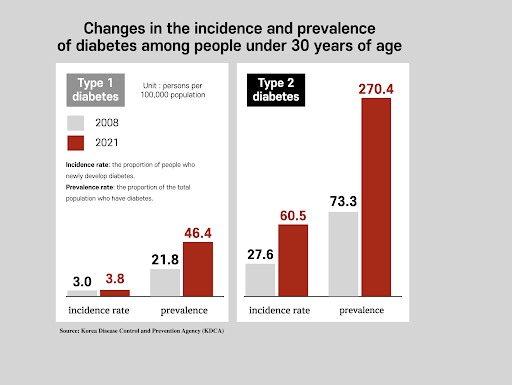
The research results released in August 2025 by the KDCA National Institute of Health are shocking. The prevalence of type-2 diabetes among people under 30 rose from 73.3 per 100,000 in 2008 to 270.4 per 100,000 in 2021, nearly a fourfold increase in just 13 years. The increase was most pronounced among adolescents aged 13 to 18.
Diseases once called “adult diseases” are now spreading rapidly among teenagers. Why is this happening?
The price paid by the ultra-processed food generation
Ultra-Processed Foods Dominate Adolescent Diets

Those born in the 1990s, 2000s, and 2010s are the first generations exposed to ultra-processed foods from birth.
Earlier generations grew up eating home-cooked meals, with fruit or rice cakes as snacks. Today’s adolescents live differently. They grab a convenience-store triangle gimbap for breakfast, barely touch their school lunch, and order fried chicken or pizza after school. Snacks consist of chips, instant noodles, and sugary sodas.
According to a 2023 survey by the Korea Food Communication Forum, ultra-processed foods account for over 35% of the average daily intake of adolescents, and for some, the proportion exceeds 50% far higher than among adults.
Physiological Vulnerability of Growing Teens
The problem is that growing adolescents are far more physiologically sensitive than adults. Excessive exposure to ultra-processed foods during the critical period when the brain and organs are developing can cause irreversible cellular-level damage. Pancreatic beta cells become depleted early, insulin resistance becomes entrenched, and plaque begins forming on blood vessel walls.
Related Article: How Ultra-Processed Foods Destroy the Gut Ecosystem
Early chronic disease means early death
Complications Appear Earlier in Children
An even more serious issue is that when diabetes begins in childhood, complications appear much earlier.
A 2024 study published in the international journal JAMA Network is alarming. Among pediatric patients with type 2 diabetes, 7% already have diabetic retinopathy, a complication that can lead to blindness. This condition typically develops after living with diabetes for 10–15 years, yet many young patients have it at the time of diagnosis.
Early-Onset Diabetes Increases Mortality Risk
The British Medical Journal forecasts an even darker future. If someone is diagnosed with type 2 diabetes before age 40, their mortality rate is up to four times higher than those diagnosed after age 40. In other words, early onset means early death.
A Generation at Risk: “Children May Die Before Their Parents.”
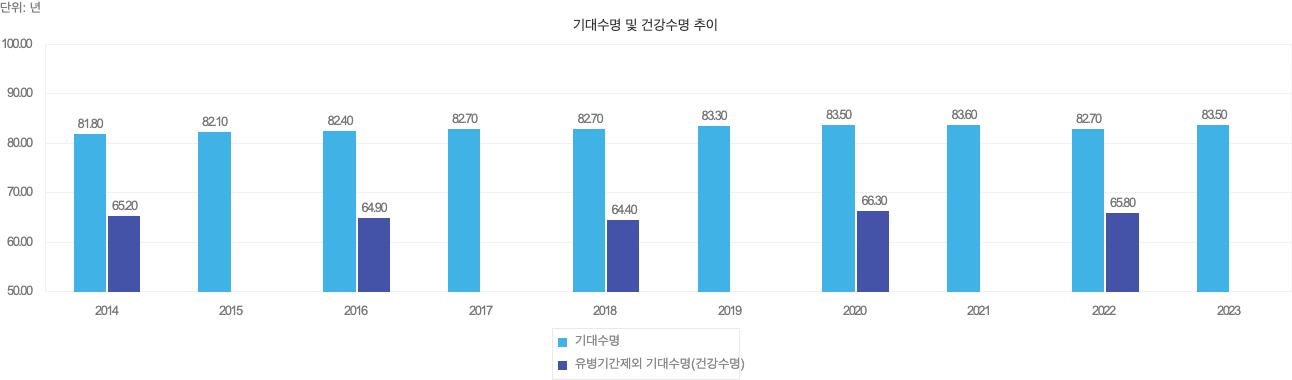
The most shocking reality is that today’s adolescents may have a shorter healthy lifespan than their parents.
According to 2023 Ministry of Health and Welfare statistics, the average life expectancy of Koreans is 83.5 years, yet the healthy life expectancy is only 66.3 years. This means the final 17 years of life are spent suffering from illness.
But today’s teenagers already have chronic diseases in their teens. Imagine their condition when they reach their 60s or 70s, or rather, will they even live that long?
A 2018 study by the Yale School of Public Health delivers a stark warning: “If the current trend of childhood obesity continues, children born in 2030 will die an average of five years earlier than their parents.”
For the first time in human history, a generation may have a shorter lifespan than the one before it.
Korea’s situation may be even worse. The rise in ultra-processed food consumption is faster than in the United States, and Korean adolescents face far higher academic stress and far less physical activity.
Poverty and Childhood Chronic Disease Risk
Income Disparities and Type-2 Diabetes Risk
Another shocking finding from the KDCA study is that income disparities translate directly into health disparities.
The risk of developing type-2 diabetes among low-income groups was 3.7 times higher than among middle- or high-income groups. Among children under 14, the gap widened to 5.1 times, and among girls, to 4.2 times.
Skipping Breakfast and Unhealthy Eating Habits
Why does this happen?
According to the National Health and Nutrition Examination Survey, the lower the income, the higher the rate of skipping breakfast. In fact, households in the lowest 20% income bracket skip breakfast at twice the rate of those in the highest 20%. Skipping breakfast leads to overeating at lunch and dinner, increasing the risk of weight gain and metabolic diseases.
Low-income families often have no choice but to rely on cheaper processed foods rather than fresh vegetables and fruits. They lack the time to cook at home and have limited access to environments where they can exercise. Poverty fuels disease, and disease then deepens poverty. A vicious cycle begins.
Park Hyun-young, Director of the National Institute of Health, warned:
“Diabetes prevalence among children and young adults continues to rise, making national-level intervention urgent. Securing health equity for socioeconomically vulnerable groups is especially critical.
This is not an individual problem

The rise of chronic diseases among adolescents is not just a matter of personal responsibility. It is a problem rooted in the social system.
Health Education and School Meals
Health education must be incorporated as a formal subject starting in elementary school. School meals should shift from ultra-processed foods to fresh, whole ingredients. Steamed or grilled dishes should replace fried foods, and natural ingredients should take precedence over processed meats.
Regulating Advertising and Improving Access to Healthy Foods
Advertising of ultra-processed foods targeting adolescents must be regulated. Junk food ads that appear indiscriminately online and on social media are a major cause of unhealthy eating habits in young people. France and the UK have already banned junk food advertising during youth viewing hours.
To reduce health inequalities in low-income households, access to fresh fruits and vegetables must be improved. Programs such as free fruit snacks in schools, support for local farmers’ markets, and healthy food vouchers are necessary.
Encouraging Physical Activity
Physical education hours should be increased, and safe spaces for children to play around schools must be created. Exercise is not just about burning calories; it is the most powerful treatment for improving insulin sensitivity and metabolic function.
Conclusion: The Choices We Make Today Determine Our Children’s Future
Choosing ultra-processed foods for convenience or taste is destroying our children’s future. The choices made at the dining table today determine their health 20 or 30 years from now.
The choice is ours.





