Hormone Replacement Therapy (HRT) remains one of the most widely discussed and researched treatments for managing menopause symptoms. For many women, it has restored a sense of well-being, easing the discomfort that often accompanies hormonal shifts during perimenopause and menopause.
While the benefits of HRT particularly when started during the early stages of menopause are well-supported by clinical evidence, it’s essential to understand that the safety and effectiveness of HRT can vary. Factors such as a woman’s age, overall health, medical history, and the type and duration of hormone therapy all play a role in determining the risk profile.
In this article, we explore:
- How Hormone Replacement Therapy Works
- The different types of HRT available
- Who is best suited for HRT treatment
- The potential benefits and risks associated with HRT
- Emerging non-hormonal alternatives like photobiomodulation therapy
By understanding these aspects, women can make informed decisions about how to manage menopause symptoms safely and effectively, whether through traditional hormone therapy or alternative approaches tailored to individual health needs.
What is Hormone Replacement Therapy?

Hormone Replacement Therapy (HRT) is a well-established medical treatment used to alleviate the symptoms associated with menopause. It works by supplementing the body with estrogen, progesterone, or a combination of both hormones, which naturally decline as women age.
Potential Benefits of Hormone Replacement Therapy
When prescribed appropriately and monitored by a healthcare professional, Hormone Replacement Therapy (HRT) can offer significant benefits that enhance both short-term well-being and long-term health outcomes for many women navigating menopause.
1. Relief from Menopausal Symptoms
HRT is widely regarded as the most effective treatment for alleviating vasomotor symptoms such as hot flashes and night sweats, which impact up to 80% of women during menopause. Beyond temperature regulation, it also helps ease vaginal dryness, painful intercourse, mood swings, and sleep disturbances—symptoms commonly associated with hormonal fluctuations during this life stage.
2. Bone Health and Osteoporosis Prevention
Estrogen is vital for maintaining bone density. After menopause, the decline in estrogen can lead to rapid bone loss up to 20% within the first 5 to 6 years. HRT helps slow this decline by preserving bone mineral density, significantly reducing the risk of osteoporosis and related fractures, including those of the spine and hip.
3. Cardiovascular Support in Younger Women
For women under 60, or those who begin HRT within 10 years of menopause, there is evidence of cardiovascular benefits. These include improved arterial function, better cholesterol balance, and a reduced risk of coronary artery disease. However, these advantages are less pronounced when HRT is initiated later in life, so timing is a critical factor.
4. Potential Protection Against Colorectal Cancer
Research suggests that combined HRT may slightly lower the risk of developing colorectal cancer. While it is not recommended solely for cancer prevention, this potential benefit may be worth considering as part of an individual’s broader health profile and risk factors.
5. Cognitive and Mood Enhancement
Emerging studies indicate that starting HRT early in the menopausal transition may support cognitive function, emotional stability, and even reduce the likelihood of developing Alzheimer’s disease. Women who experience brain fog, memory lapses, or mood changes tied to hormonal shifts may find relief with appropriately timed HRT.
Potential Risks of Hormone Replacement Therapy
Hormone Replacement Therapy (HRT) can provide substantial benefits, especially for managing menopausal symptoms. However, like any medical treatment, it comes with potential risks. Understanding these risks—who they affect and how they’re influenced by factors such as age, health status, and the type of HRT is key to making informed decisions.
1. Breast Cancer
One of the most well-publicized concerns about HRT is its potential link to breast cancer. Research shows that long-term use of combined HRT (estrogen plus progestin) may slightly increase the risk, particularly after more than five years of use. However, estrogen-only HRT, typically prescribed to women who’ve had a hysterectomy, does not significantly raise breast cancer risk and may even reduce it, as suggested by some findings from the Women’s Health Initiative (WHI). Importantly, breast cancer risk tends to decline once HRT is discontinued.
2. Blood Clots (Deep Vein Thrombosis and Pulmonary Embolism)
Oral estrogen, especially in pill form, has been shown to increase the risk of blood clots, such as deep vein thrombosis (DVT) and pulmonary embolism (PE). This is because oral hormones pass through the liver, where they can alter clotting mechanisms. Transdermal estrogen (patches, gels, sprays), which bypasses the liver, carries a much lower risk of clot formation, making it a preferred option for women at higher clotting risk.
3. Stroke
The risk of ischemic stroke may also increase with HRT, particularly for women who begin treatment after age 60 or have existing cardiovascular risk factors. However, when HRT is started within 10 years of menopause onset, especially via non-oral routes, the stroke risk appears to be minimal.
4. Heart Disease
The relationship between HRT and cardiovascular disease is complex. Initial WHI findings suggested an increased risk of heart disease, but further analysis led to the development of the “timing hypothesis.” This hypothesis proposes that starting HRT early in menopause (before age 60 or within 10 years of the last period) may offer cardioprotective benefits. Conversely, starting HRT later in life, particularly in women with existing heart conditions, may elevate the risk of heart attacks and other cardiac events.
5. Gallbladder Disease
Lastly, gallbladder issues, such as the formation of gallstones and the need for gallbladder surgery, have been linked to oral estrogen therapy. As with clotting risks, this side effect is significantly reduced with transdermal HRT, reinforcing the importance of selecting the appropriate delivery method based on individual risk factors.
Who Should and Shouldn’t Consider HRT?
Hormone Replacement Therapy (HRT) isn’t a one-size-fits-all solution. Whether it’s appropriate depends on your individual health profile, medical history, and stage of menopause. Some women are ideal candidates, while for others, the risks may outweigh the benefits.
You may be a good candidate for HRT if:
- You are under 60 years old or within 10 years of menopause
- You experience moderate to severe menopausal symptoms, such as hot flashes, night sweats, or vaginal dryness
- You have a low risk of breast cancer, blood clots, or cardiovascular disease
HRT may not be suitable if:
- You have a history of breast, ovarian, or endometrial cancer
- You’ve had a stroke, a blood clot, or a heart attack
- You suffer from liver disease or uncontrolled high blood pressure
- You are over 60 and considering HRT for the first time
No matter your situation, a personalized risk-benefit assessment with your doctor is essential before starting HRT.
Alternatives To Hormone Replacement Therapy
Hormone Replacement Therapy isn’t the only way to manage menopause symptoms.
Whether you’re unable to take HRT or simply prefer a different approach, several non-hormonal options can offer relief.
1. Non-Hormonal Medications:
These prescription treatments can help alleviate specific menopause symptoms:
- SSRIs and SNRIs (e.g., venlafaxine): Originally used as antidepressants, they can reduce hot flashes and improve mood.
- Gabapentin: Commonly prescribed for nerve pain, it can help with night sweats and improve sleep quality.
- Clonidine: Typically used for high blood pressure, it may lessen hot flashes, though it tends to be less effective than other options.
- Ospemifene: A non-estrogen medication designed to treat vaginal dryness and painful intercourse.
Natural Alternatives To Hormone Replacement Therapy
- Exercise: Improves mood, sleep, bone strength, and heart health
- Healthy diet: Rich in calcium, vitamin D, and phytoestrogens (like soy)
- Quit smoking and limit alcohol
- Cognitive Behavioral Therapy (CBT): Shown to help with sleep and emotional symptoms
- Mindfulness, yoga, acupuncture: May help relieve stress and improve well-being
Always check with your doctor before starting supplements or herbal remedies like black cohosh, which may interact with medications.
Lifestyle changes and holistic approaches may offer symptom relief without medication:
- Exercise: Regular physical activity boosts mood, enhances sleep, strengthens bones, and supports cardiovascular health.
- Balanced Diet: Eat foods rich in:
- Calcium and Vitamin D: For bone health
- Phytoestrogens (found in soy, flaxseeds, and legumes): Plant-based compounds that may mimic estrogen in the body
- Avoid Smoking and Limit Alcohol: Both can worsen menopause symptoms and increase health risks.
- Cognitive Behavioral Therapy (CBT): Proven to help with insomnia, anxiety, and mood swings during menopause.
- Mind-Body Practices:
- Mindfulness & Yoga: Reduce stress and promote emotional well-being.
- Acupuncture: Some women find it beneficial for managing hot flashes and anxiety.
Important Note: Before taking any supplements or herbal remedies like black cohosh, always consult your doctor. Some natural products can interact with medications or cause unwanted side effects.
Photobiomodulation Therapy: A Safe and Natural Alternative to Hormone Replacement Therapy

Photobiomodulation (PBM) therapy harnesses the power of specific red and near-infrared light wavelengths to stimulate cellular energy, enhance mitochondrial function, and promote systemic physiological balance.
Recent studies indicate that PBM may support hormonal health by naturally influencing key endocrine glands such as the thyroid, adrenal, and pineal glands, offering a gentle yet effective approach to hormonal regulation.
Emerging evidence suggests that PBM may help:
- Naturally boosts testosterone and estrogen levels
- Enhances energy, mood, and quality of sleep
- Improves libido and overall sexual wellness
- Reduces inflammation and accelerates cellular repair
Unlike traditional Hormone Replacement Therapy (HRT), which introduces synthetic hormones into the body, PBM encourages your body’s own ability to regulate hormones safely and non-invasively. It is a drug-free therapy suitable for consistent, long-term use.
“Ready to Explore PBM?”
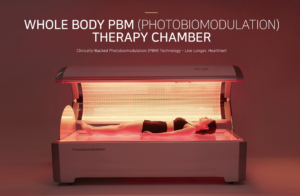
Connect with our specialists to learn how PBM therapy can support your hormonal and overall health. Browse our advanced PBM devices designed to restore balance from within and empower your well-being naturally.[/vc_column_text][/vc_column][/vc_row]












