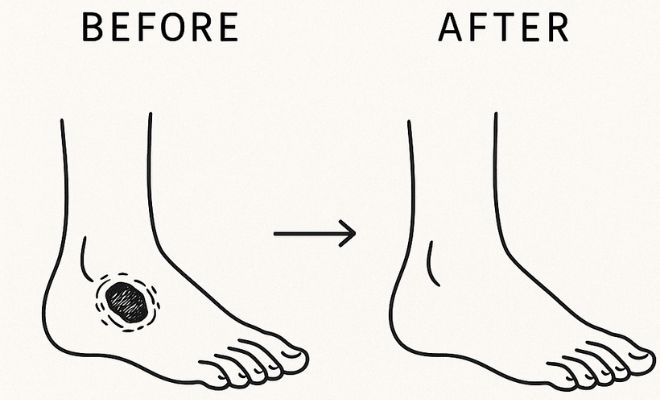
Diabetic foot ulcers (DFUs) are not just a common side effect of poorly managed diabetes; they’re a serious medical crisis. Research suggests that roughly 15 to 20% of people with diabetes will develop a foot ulcer during their lifetime. These wounds are notoriously difficult to heal due to poor blood flow, nerve damage, and a compromised immune response. In fact, up to 85% of diabetes-related amputations begin with an ulcer that fails to heal.
While conventional treatments like debridement, antibiotics, and offloading remain the cornerstone of care, many chronic wounds don’t respond adequately. That’s where Hyperbaric Oxygen Therapy (HBOT) comes in.
Let’s explore why HBOT is gaining attention as a powerful adjunct therapy and how it could be a limb-saving solution for high-risk diabetic patients.
Understanding Diabetic Foot Wounds

Diabetic foot ulcers stem from a combination of factors that impair the body’s ability to heal wounds effectively:
- Peripheral Neuropathy: Nerve damage reduces sensation in the feet, allowing injuries to go unnoticed and worsen over time.
- Peripheral Arterial Disease (PAD): Reduced blood flow limits oxygen and nutrient delivery to tissues, hindering healing.
- Impaired Immune Response: Diabetes weakens the immune system, increasing the risk of infection in wounds.
These issues combine to create a dangerous situation, where even a small cut or blister on the foot can turn into a serious, long-lasting wound. If not properly treated, it can lead to gangrene and may even require amputation. In fact, foot problems caused by diabetes are one of the top reasons people lose limbs around the world.
What Is Hyperbaric Oxygen Therapy (HBOT)?
HBOT is a medical treatment that involves inhaling 100% pure oxygen in a pressurized environment, typically at 2.0 to 2.5 atmospheres absolute (ATA). That’s more than twice the atmospheric pressure at sea level.
Why Pressure Matters
Under normal conditions, oxygen is carried almost exclusively by red blood cells. But in a pressurized chamber, oxygen dissolves directly into the plasma, lymph fluid, and other body compartments. This increases oxygen delivery by 10–15 times, especially to areas where blood flow is impaired, like DFUs. The result is a dramatic and immediate boost in tissue oxygenation, allowing for enhanced cellular activity, faster healing, and improved infection control.
How HBOT Helps Diabetic Foot Ulcers Heal
1. Increases Oxygen Delivery to Hypoxic Tissue
Most chronic foot ulcers are hypoxic, meaning they lack adequate oxygen to sustain healing. Normal healing processes, like inflammation, tissue remodeling, and angiogenesis, all require oxygen.
- HBOT bypasses the need for functional blood vessels by delivering oxygen directly into tissue fluids.
- Oxygen gradients created during therapy persist for several hours after treatment, creating a favorable environment for tissue repair.
Example: In a DFU with poor peripheral circulation, red blood cells may not reach the area, but dissolved oxygen from plasma still can. That’s the advantage of HBOT.
2. Stimulates Angiogenesis
HBOT promotes the formation of new blood vessels (angiogenesis) by stimulating the release of growth factors like vascular endothelial growth factor (VEGF). These new vessels improve long-term blood supply to the wound site, creating a sustainable environment for healing even after HBOT sessions conclude.
Clinical relevance: A randomized trial published in Wound Repair and Regeneration showed that patients receiving HBOT had significantly greater capillary density in ulcerated tissue than controls after just 20 sessions.
3. Promotes Collagen Synthesis and Cell Regeneration
Oxygen is a critical component of wound healing, as it fuels fibroblast activity (cells responsible for tissue repair), collagen production, and epithelialization (the formation of new skin). HBOT enhances these processes, strengthening the structural integrity of newly formed tissue and accelerating wound closure. This means stronger, more resilient tissue forms over the wound.
4. Boosts Immune Function
Infection is one of the biggest barriers to healing diabetic ulcers. HBOT strengthens the immune system by:
- Enhancing leukocyte oxidative killing (white blood cells use oxygen to kill bacteria)
- Improving macrophage function, which clears debris and pathogens
- Reducing bacterial growth, especially anaerobic organisms like Clostridium species
Oxygen also supports the antibiotic effect of certain drugs, improving their penetration and efficacy in infected tissues.
5. Reduces Inflammation and Edema
When a wound stays inflamed and swollen, it slows down healing. That’s because inflammation blocks blood flow and stops oxygen and nutrients from reaching the damaged tissue. Hyperbaric Oxygen Therapy (HBOT) helps by calming inflammation and reducing fluid buildup (also known as edema).
Here’s how HBOT supports healing:
- It turns down harmful inflammation signals like TNF-α and IL-1β
- It boosts natural anti-inflammatory compounds in your body
- It makes blood vessels less leaky, which helps stop extra fluid from collecting in tissues
With less swelling, there’s better blood flow, less pain, and faster healing. HBOT helps move stubborn, chronic wounds out of the stuck “inflammation mode” and into active recovery.
Related Article: Hyperbaric Chamber for Lyme Disease
Clinical Evidence Supporting HBOT for DFUs
The efficacy of HBOT is backed by robust clinical evidence:
- A 2013 Cochrane Review found HBOT significantly improved healing rates and reduced amputation risk in patients with DFUs, especially when combined with standard care.
- A double-blind randomized trial (Löndahl et al., 2010) found that 52% of patients receiving HBOT achieved complete healing vs. only 29% in the control group.
- HBOT is FDA-approved for Wagner Grade 3 or higher diabetic wounds that haven’t healed after 30 days of conventional treatment.
In practical terms, this means HBOT is not experimental; it’s a medically validated, life- and limb-saving treatment when used appropriately.
What to Expect During Treatment
A typical HBOT protocol includes:
- Treatment sessions: 90 to 120 minutes per session
- Frequency: 5 days per week
- Total sessions: 20–40 initially; more may be added based on progress
Patients lie in a chamber and breathe oxygen while pressure is gradually increased. Many describe it as painless and relaxing.
Monitoring: Medical personnel continuously monitor vitals and oxygen saturation. Progress is often tracked with photographic wound measurements and tissue oxygen levels.
Risks and Side Effects
HBOT is remarkably safe, but potential side effects include:
- Ear or sinus barotrauma (pressure-related discomfort)
- Temporary vision changes due to lens refraction
- Claustrophobia (single-person chambers may feel confining)
- Rare events: Oxygen toxicity (causing seizures) is extremely uncommon when proper protocols are followed
In most clinical settings, risk mitigation includes slow pressurization, patient screening, and close observation.
Get Started With Huelight’s Medical Grade HBOT Device
If you or a loved one is dealing with a stubborn diabetic foot ulcer that hasn’t responded to standard treatments, Hyperbaric Oxygen Therapy offers real hope. As we’ve seen, HBOT not only accelerates wound healing, but it also addresses the root problems of poor circulation, oxygen deprivation, and chronic inflammation that make diabetic wounds so difficult to treat.
HueLight’s HBOT Device is specifically engineered for serious clinical applications like diabetic foot ulcers. With a powerful pressure range of up to 3.0 ATA, it delivers far more oxygen than standard home-use chambers, making it ideal for chronic, non-healing wounds that need intensive support.
Built with hospital-grade materials, Huelight’s HBOT offers:
- A full-length, ergonomic bed design for maximum patient comfort
- Dual touchscreen controls (interior + exterior) for safety and flexibility
- Real-time monitoring and two-way communication
- FDA-recognized oxygen delivery in a sealed, medical-grade environment
Whether you’re a clinic treating diabetic patients or an individual seeking long-term healing support, HueLight’s HBOT Device is a high-performance solution backed by science, safety, and global medical certifications.
Don’t wait for ulcers to escalate, take proactive action.
Contact us to book your Hyperbaric Oxygen Therapy Device today!
Related Article: Hyperbaric Oxygen Therapy at Home: Is It Right for You?