The Gut-Brain Connection: A New Frontier in Parkinson’s Research
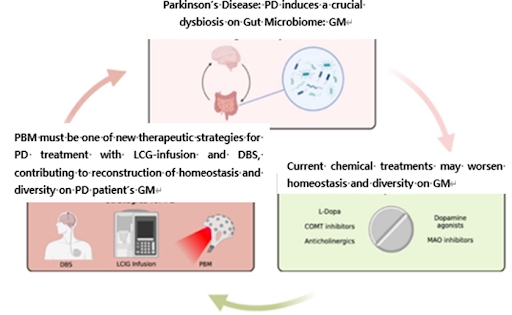
Parkinson’s disease is difficult to regard as solely a brain disorder. Recent research continues to support the deep connection between neurodegeneration and the gut microbiome — a concept known as the Gut–Brain Axis.
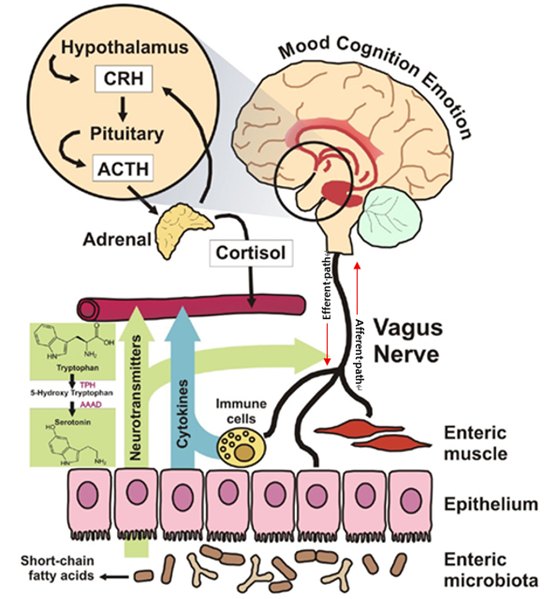
This axis is composed of:
CNS (Central Nervous System)
ENS (Enteric Nervous System)
VNS (Vagus Nerve)
These systems are in constant bidirectional communication. Among them, the gut microbiota influences this axis by regulating neural signaling, immune responses, and hormone metabolism. Disruptions here may hold clues to Parkinson’s origins and potential treatments.
What Does Gut Microbiota Imbalance Have to Do with Parkinson’s Disease?
One of the common symptoms observed in Parkinson’s patients is indigestion, constipation, and leaky gut syndrome. Many Parkinson’s patients experience digestive issues years before motor symptoms appear. Science now suggests this is no coincidence:
These may appear to be mere digestive issues, but in reality, gut dysbiosis (microbial imbalance) is one of the major causes.
Numerous studies have found that:
Bacterial species reduced in healthy individuals: Prevotella, Roseburia, Blautia, Faecalibacterium
Bacterial species increased in Parkinson’s patients: Akkermansia, Lactobacillus
Among these, Roseburia, Faecalibacterium, and Blautia produce short-chain fatty acids (SCFAs) that protect the intestinal lining, suppress inflammation, and regulate immune function. However, Parkinson’s patients show a significant reduction in these beneficial bacteria, with a corresponding increase in potentially pro-inflammatory microbes.
Why This Matters:
The depleted bacteria normally produce short-chain fatty acids (SCFAs) that:
→ Strengthen the intestinal lining
→ Reduce inflammation
→ Support immune function
Could the Origin of the Disease Be the Gut, Not the Brain?
Recent studies have proposed a hypothesis that abnormal accumulation of a protein called alpha-synuclein (α-synuclein) may begin in the enteric nervous system (ENS) and then travel along the vagus nerve to the central nervous system, potentially triggering Parkinson’s disease.
In conclusion, gut health is brain health, and restoring the balance of the gut microbiota may be a crucial key in treating Parkinson’s disease, as supported by multiple studies.
So, Where Is the Answer?
The answer may lie in whole-body PBM therapy.
PBM (Photobiomodulation) therapy uses light energy to activate cells. Recent research shows that whole-body PBM also has a significant impact on restoring gut microbiota balance. PBM can be used as a new Therapeutic strategy for Parkinson’s patients and patients with borderline early symptoms of Parkinson’s disease, prospectively.
Scientific Basis: Whole-Body PBM Revives the Gut Microbiota
According to a study by Dr. Bicknell in the UK, the following changes were observed after whole-body PBM treatment like the followings.
- Increase in beneficial bacteria such as Lactobacillus, Bifidobacterium, and Faecalibacterium
- Decrease in harmful bacteria and improvement of inflammatory conditions in the gut
- Stabilization of the mucus layer (a jelly-like layer that protects the intestinal lining) → protection of the intestinal lining → restoration of the gut–brain axis
The Result?
These effects enable healthy signal transmission between the brain, gut, and autonomic nervous system and may help normalize the dopaminergic system. Meaning improved gut-brain communication and potential dopaminergic system normalization, crucial for Parkinson’s management.
Picture of Whole Body-Photobiomodulation; WB-PBM [Ref. Hue Light Medical Research Centre]
Who Could Benefit from This?
- Individuals with Parkinson’s disease or early signs of autonomic nervous system dysfunction
- Individuals experiencing indigestion, constipation, or leaky gut syndrome
- Those looking for new treatment options beyond medication
- People seeking to improve both immune function and nervous system regulation
Conclusion: Whole-Body PBM Therapy Heals the Gut and Protects the Brain
Parkinson’s disease is not just a disorder of the brain.
Our gut and gut microbiota may be the starting point of the disease and the key to recovery.
Whole-body Photobiomodulation (PBM) therapy stands out as a dual-action solution:
1️⃣ Gut Restoration: Clinically shown to rebalance microbiota, reduce inflammation, and strengthen the intestinal barrier
2️⃣ Neural Support: Enhances communication along the vagus nerve while promoting dopaminergic health
Unlike conventional approaches, PBM offers:
✓ Non-invasive application
✓ No pharmaceutical side effects
✓ Whole-body benefits beyond symptom management
The Future of Parkinson’s Care may lie in this innovative intersection of light therapy, gut health, and neurology, offering new hope where traditional treatments fall short.
For those exploring comprehensive Parkinson’s management, whole-body PBM presents a scientifically backed pathway worth discussing with your healthcare provider.
Reference
- Bicknell et al., Microbiome Changes in Humans with Parkinson’s Disease after Photobiomodulation Therapy: A Retrospective Study. J Pers Med. 2022. 5;12(1):49. https://doi.org/10.3390/jpm12010049
- Hey et al., Therapy for Parkinson’s disease and the gut microbiome: evidence for bidirectional connection. 2023. Front. Aging Neurosci. 15:115180. https://doi.org/10.3389/fnagi.2023.1151850
- Salim S. et al., Gut microbiome and Parkinson’s disease: Perspective on pathogenesis and treatment. 2023. J Adv Res. 50:83-105. https://doi.org/10.1016/j.jare.2022.10.013
- Hakimiha N. et al., Photobiomodulation and the oral-gut microbiome axis: therapeutic potential and challenges. Front. Med. 12:1555704. https://doi.org/10.3389/fmed.2025.1555704
- Ailioaie L.M. and Litscher G., Probiotics, Photobiomodulation, and Disease Management: Controversies and Challenges. 2021. Int. J. Mol. Sci. 22:4942. https://doi.org/10.3390/ijms22094942