“Depression is not an illness of the mind. It is a collapse of the biological system.”
According to 2024 statistical data, over 1.1 million people in Korea were diagnosed with depression, marking a 33% increase in just five years. Nearly 40% of adults experienced depressive symptoms lasting several days. The World Health Organization (WHO) predicts that by 2030, depression will become the leading cause of global disease burden.
Yet society often says things like: “It’s because your mind is weak,” or “You lack willpower.” While media outlets promote mindfulness, positive thinking, and mental care programs, the truth is far more complex. Depression is a mental illness, a medical condition with biological roots, not a sign of personal failure. Research now shows that the biological causes of depression, not moral weakness, are often at the root. Understanding these causes of depression is essential to effective treatment and prevention.
Why Biological Depression Matters
Depression is often seen as an emotional or psychological issue, but modern science has revealed a deeper truth: it begins inside the body long before it reaches the mind. When key biological systems malfunction, your mood, motivation, and energy drop as predictable physiological responses, not personal failures. Depression frequently co-occurs with other mental disorders, such as anxiety or substance use disorders, making it a complex and multifaceted condition.
Understanding these biological processes is essential because treating depression at its root requires restoring the systems that have collapsed, not relying solely on willpower, mindset, or talk therapy.
Quick Overview: 4 Biological Causes of Major Depressive Disorder
- Broken Circadian Rhythm: The brain’s master clock misfires, disrupting sleep, serotonin, dopamine, and hormone balance.
- Mitochondrial Shutdown: Brain cells fail to produce energy, leading to fatigue, brain fog, and lack of motivation.
- Chronic Inflammation: Immune cells attack the brain, reducing serotonin and damaging emotional regulation centers.
- Gut–Brain Axis Collapse: Gut bacteria stop producing serotonin, directly affecting mood and cognitive function.
Depression Is a Biological Collapse, Not a Weak Mind
Depression is often misunderstood as a failure of the mind or a lack of willpower. The latest research reveals that depression is a biological catastrophe, in which four critical systems in the brain and body collapse in sequence. When these systems break down, it causes depression at a physiological level by disrupting neuroplasticity, neurotransmitter balance, and metabolic activity in key brain regions.
- Circadian Rhythm (Brain Clock)
- Mitochondria (Power Plants of Brain Cells)
- Chronic Inflammation (Immune System Conflict)
- Gut–Brain Axis (Happiness Factory)
Other biological and environmental factors associated with depression include genetic predisposition, oxidative stress, sleep disturbances, and exposure to chronic stressors.
When the biological features of depression are compared to other mood states or disorders, depression shows distinct patterns of metabolic activity and structural changes in brain regions such as the subgenual cingulate, prefrontal cortex, amygdala, and hippocampus.
Understanding these biological causes of depression is key to effective treatment and prevention.
What Are the Biological Causes of Depression?
System 1: The clock inside the brain has stopped (Circadian Rhythm)
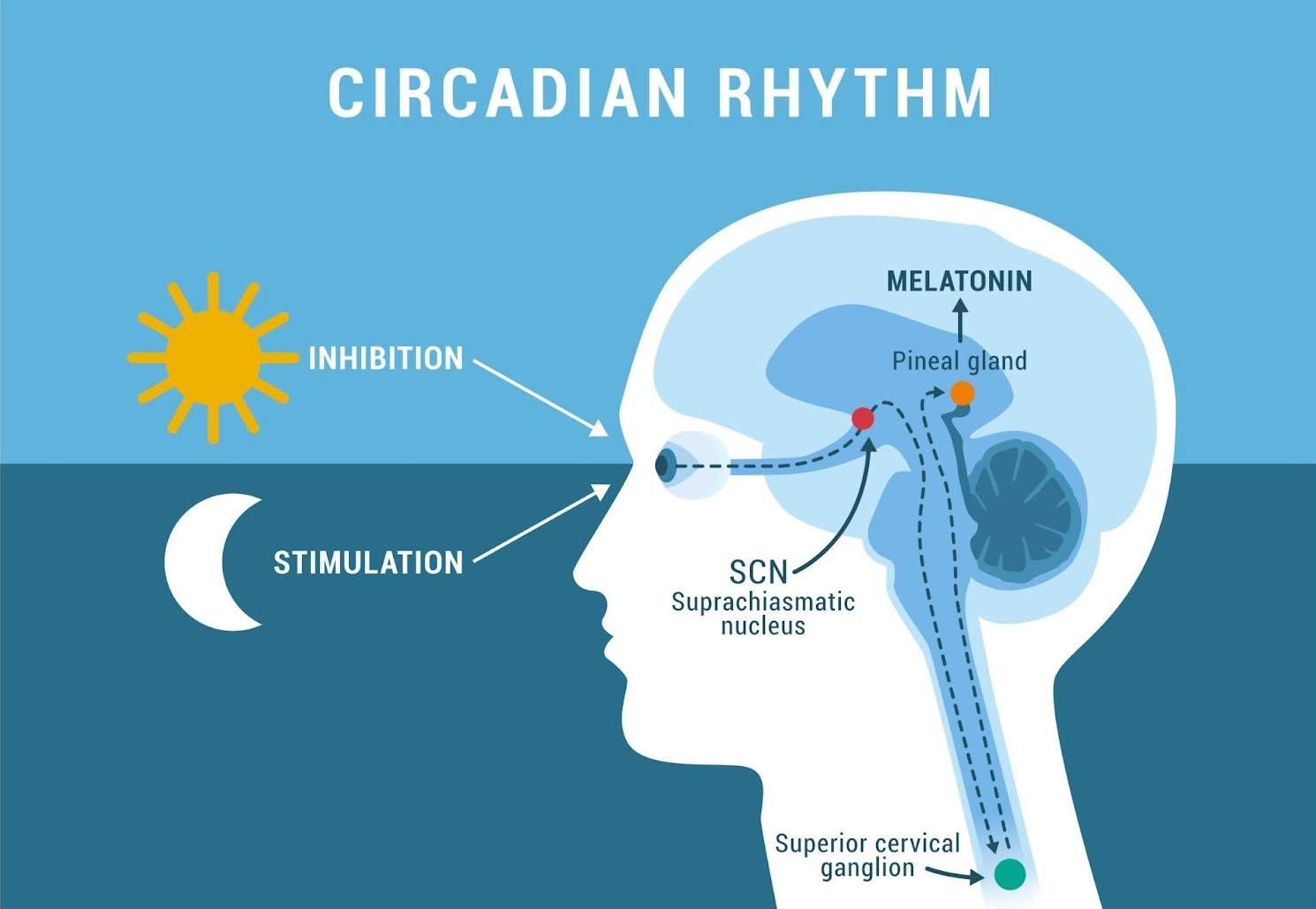
Deep inside the brain, in the hypothalamus, there is a rice-grain-sized “master clock” (SCN). This clock is the conductor that instructs the body to release energizing hormones during the day and sleep hormones at night.
According to a recent study (eBioMedicine, 2024), people with depression do not become depressed because they can’t sleep. They become depressed because the clock breaks first. Sleep deprivation can further disrupt circadian rhythms and worsen depressive symptoms. Conditions like seasonal affective disorder are also linked to disruptions in circadian rhythms and serotonin regulation.
When you stay up late staring at a smartphone and exposing yourself to light, the brain’s clock mistakes it for daytime. The result is disastrous. Serotonin, the “happiness hormone,” and dopamine, the “motivation hormone,” are released at the wrong time or dry up completely. Selective serotonin reuptake inhibitors are commonly used to manage mood disorders by influencing serotonergic activity and sleep patterns.
A brain with a broken clock is not simply tired. Lost in confusion about when to sleep and when to wake, it shuts down the very instinct for survival.
System 2: The power plants of brain cells have shut down (Mitochondria)
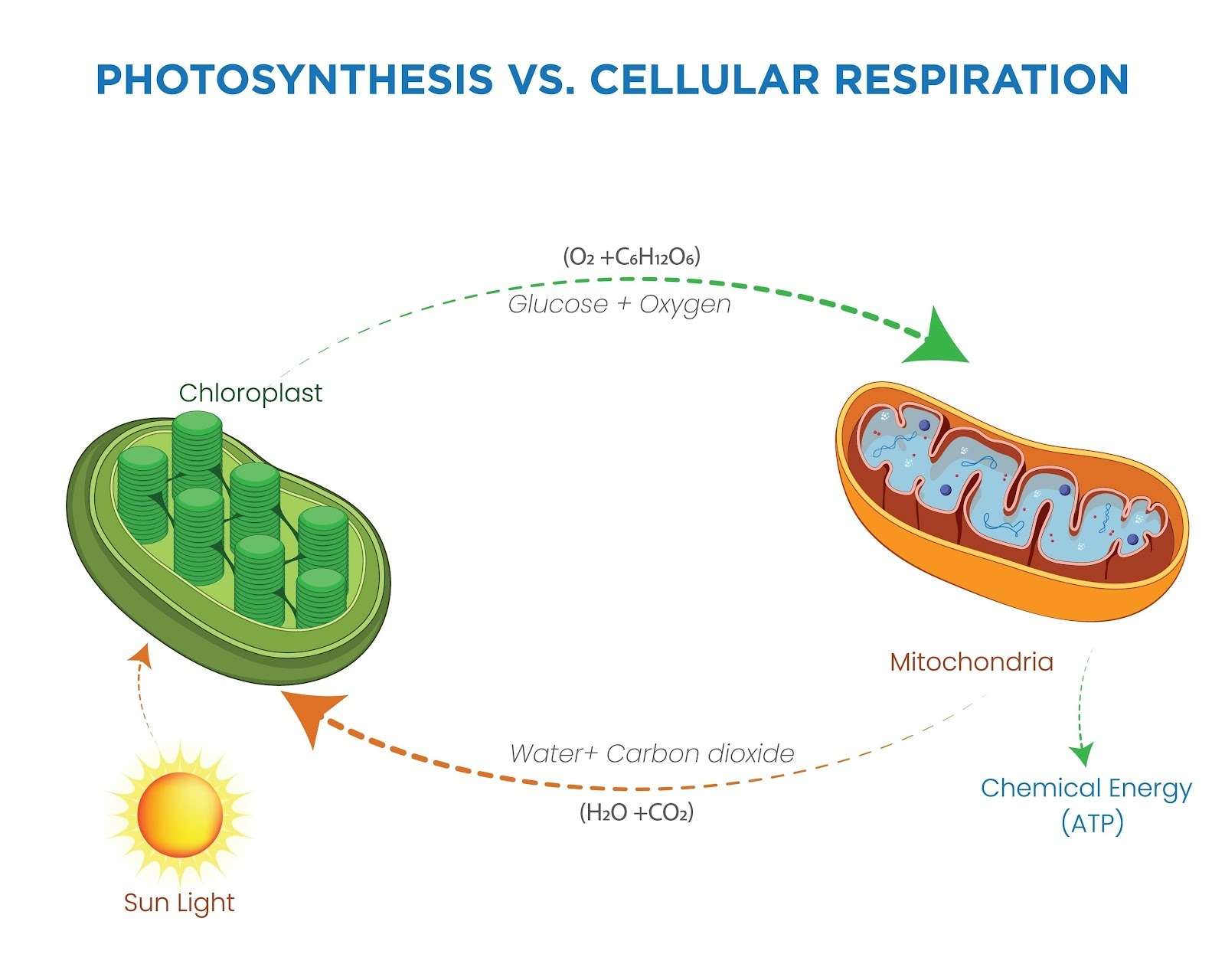
The brain accounts for only 2% of body weight, yet it consumes 20% of the body’s total energy. The place that produces this massive amount of energy is the tiny power plant inside each cell, the mitochondria.
Have you ever felt like “there’s a fog in your head (Brain Fog)”? This is not just a mood. According to real research (CNS Neuroscience & Therapeutics, 2024), the power plants in the brain cells of people with depression are old and damaged.
Just as a car cannot run without fuel, the brain cannot generate any motivation if the mitochondria cannot produce energy (ATP). It is not that you lack willpower. Your brain simply has no fuel left to operate.
System 3: A civil war has broken out inside the brain (Chronic Inflammation and Chronic Stress)
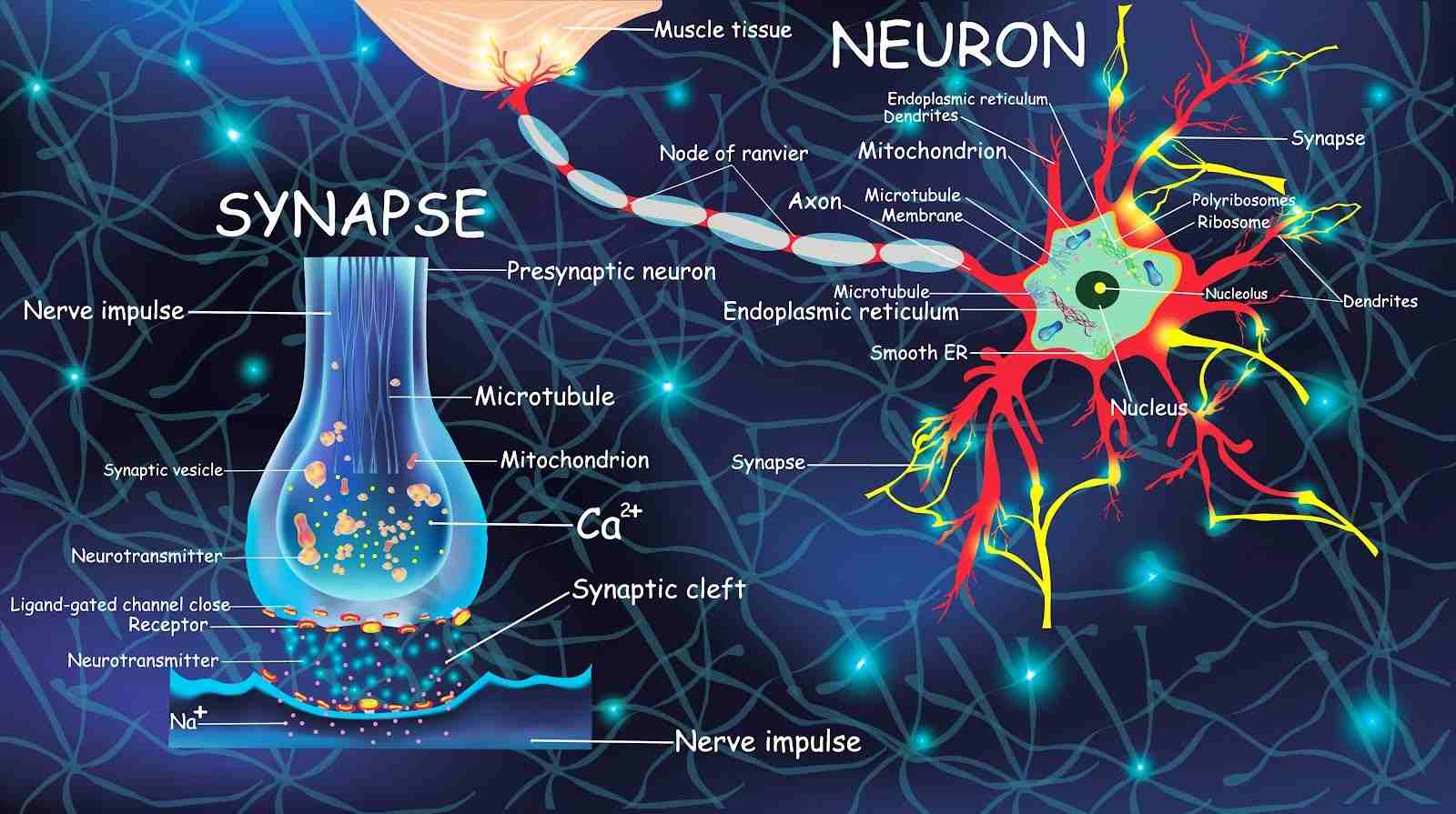
When the power plants (mitochondria) break down, fragments spill out. The body’s immune cells mistake these fragments for “enemy forces” and launch attacks. An “inflammatory war” begins inside the brain. Uncontrolled stress can trigger or worsen this inflammation, leading to further disruption of brain function and contributing to depressive symptoms.
These inflammatory substances are highly intelligent villains.
- Happiness theft: They intercept and eliminate the raw materials needed to produce serotonin, the happiness hormone.
- Memory destruction: They shrink the hippocampus, the key region that regulates memory and emotion.
In 2024, the academic community identified “uncontrolled inflammation destroying neuronal communication systems” as the core mechanism of depression. When the brain is on fire, positive thinking alone cannot extinguish the flames.
System 4: The happiness factory has gone on strike (Gut–Brain Axis)
Surprisingly, 90% of serotonin, the happiness hormone, is produced not in the brain but in the gut. The 100 trillion microorganisms living in your intestines are the workers that manufacture it.
But when you experience stress or your diet collapses, beneficial gut bacteria disappear and harmful, toxin-producing bacteria take over. Lifestyle factors such as diet, sleep, and physical activity can significantly influence gut health and increase or decrease the risk of depression. Environmental factors, including exposure to toxins or chronic stress, can also disrupt the gut microbiome and contribute to depression. Many non-genetic factors, such as adverse experiences and lifestyle choices, play a significant role in the development of depression through their impact on the gut–brain axis. When the happiness factory goes on strike, the supply of happiness meant to be delivered to the brain gets cut off.
There is even a shocking experiment showing that when stool from a patient with depression was transplanted into a healthy mouse, the mouse began to exhibit depressive symptoms. This proves that “the collapse of the gut is the collapse of mood.
Genetic Vulnerability: The Blueprint of Risk
When it comes to major depressive disorder, your genetic makeup can play a powerful role in shaping your risk. Studies consistently show that individuals with a family history of depression are more likely to experience depressive symptoms themselves. This increased risk is not just a matter of chance; genetic factors can influence how your brain responds to stress, how neurotransmitters function, and even how your body manages inflammation.
But genetics are only part of the story. The development of major depression is often the result of a complex interplay between your inherited blueprint and the environment you grow up in. Early life stress, chronic stress, and traumatic life events such as childhood adversity or significant losses can all interact with your genetic vulnerability, making some people more prone to developing depressive disorders than others.
Genetic differences help explain why some individuals develop depression after stressful life events, while others remain resilient. For example, certain gene variants may make the brain’s stress system more sensitive, increasing the likelihood of depressive symptoms when faced with environmental challenges. This means that both your family history and your life experiences contribute to your overall risk for depression.
Understanding your genetic vulnerability is not about assigning blame or feeling powerless. Instead, it highlights the importance of recognizing depression as a multifaceted condition, one that arises from the dynamic relationship between your genes and your environment. By acknowledging these risk factors, you can work with a mental health professional to develop personalized strategies for prevention, early intervention, and effective treatment.
Depression Symptoms of Biological Depression
Recognizing the symptoms of depression early, which often result from underlying biological changes, can help in timely intervention. Common signs include:
- Persistent fatigue and brain fog: Feeling constantly tired and mentally sluggish, even after adequate rest.
- Loss of motivation and pleasure: Losing interest in activities that used to be enjoyable, along with difficulty initiating tasks.
- Difficulty sleeping or irregular sleep patterns: Experiencing insomnia, restless sleep, or sleeping at unusual times.
- Mood swings and irritability: Frequent changes in mood, increased frustration, or emotional sensitivity.
- Digestive issues linked to gut imbalance: Experiencing bloating, constipation, diarrhea, or other gastrointestinal problems due to a disrupted gut microbiome.
These are the depression symptoms observed in both clinical and experimental settings. Depressive behaviors, such as reduced motivation and anhedonia, are also studied in animal models to better understand the biological basis of depression.
How Lifestyle Factors Influence Biological Depression
Lifestyle habits play a major role in either worsening or improving biological depression. Small daily behaviors can directly impact the brain, mitochondria, gut microbiome, and hormones, and can either increase or decrease depression risk depending on the choices made. Here’s how:
- Sleep: Maintaining regular sleep and wake times helps restore the circadian rhythm, which regulates mood, energy, and hormonal balance. Poor sleep disrupts neurotransmitter production and can intensify depressive symptoms.
- Diet: Eating foods rich in prebiotics and probiotics, such as yogurt, kefir, kimchi, bananas, or whole grains, supports the gut microbiome. Since the gut produces key neurotransmitters like serotonin, a healthier gut can reduce inflammation and improve overall mood.
- Exercise: Even mild physical activity, like walking or stretching, boosts mitochondrial energy production. Better mitochondrial function leads to improved mood stability, reduced fatigue, and stronger stress resilience.
- Stress Management: Practices like mindfulness, deep breathing, journaling, or meditation help lower stress hormones and chronic inflammation. Over time, these habits strengthen the nervous system and reduce the biological triggers that contribute to depression, lowering the likelihood of developing depression.
Additionally, lifestyle improvements can support psychological well-being by addressing low self-esteem, which is a known risk factor for depression.
Advanced Scientific Treatments for Depression
For severe cases, scientific interventions may be necessary:
- PBM (Photobiomodulation) Therapy: Activates mitochondria using specific light wavelengths and can stimulate nerve cell growth, which is important for recovery from depression.
- Oxygen and Hydrogen Therapy: Reduces neuroinflammation and restores cellular energy.
This is not a simple mechanical treatment. It is the most fundamental biological rebooting process, restarting a stopped biological clock and reigniting the power plants that have gone dark.
Differences Between Biological and Psychological Depression
| Aspect | Biological Depression | Psychological Depression |
| Cause | Physiological breakdown (brain, mitochondria, inflammation, gut). The traditional ‘chemical imbalance’ theory, especially involving serotonin, is now considered overly simplistic and not fully supported by scientific evidence; depression involves complex neurotransmitter and neuronal changes. | External stressors or trauma. Psychological factors such as rumination, negative self-concept, neuroticism, and emotional clarity play a key role in increasing vulnerability to depression. Negative affective biases in emotional processing also contribute to the development and maintenance of depressive symptoms |
| Treatment | Lifestyle + scientific interventions | Counseling, therapy |
| Key Difference | Positive thinking alone is insufficient | Can improve with cognitive techniques |
Prevention Tips for Biological Depression
Simple daily habits can go a long way in supporting your brain, gut, and overall biology. Here are effective prevention strategies that can help prevent depression and reduce the risk of both initial and recurrent episodes:
-
Maintain consistent sleep schedules:
Going to bed and waking up at the same time each day helps regulate your circadian rhythm, stabilizing mood, energy, and hormonal balance. Consistency can significantly reduce biological stress on the body. Maintaining healthy sleep habits can also lower the risk of experiencing a major depressive episode.
-
Eat a balanced diet rich in gut-friendly foods:
Include fiber-rich vegetables, fermented foods, and omega-3 sources to nourish your gut microbiome. A healthy gut directly supports neurotransmitter production and reduces inflammation linked to biological depression. Good nutrition is also associated with a reduced likelihood of major depressive episodes.
-
Avoid late-night screen exposure:
Blue light from phones and laptops disrupts melatonin production, making it harder for your brain to wind down. Reducing screen use at night helps improve sleep quality and supports emotional regulation.
-
Exercise regularly:
Even light physical activity increases blood flow, boosts endorphins, and supports mitochondrial health. Regular movement is one of the most effective ways to protect your brain and body from depressive symptoms. Exercise is also important for prevention, as it can reduce the risk of recurrent depression.
-
Manage stress with meditation or therapy:
Practices like mindful breathing, meditation, or cognitive-behavioral therapy help reduce chronic stress, which is a key driver of biological imbalance. These habits strengthen emotional resilience and nervous system function, and play a role in preventing depression.
Conclusion: This is not “Morality”; it is “science.”
No one tells a person with a broken leg, “Walk using your willpower.” The same applies to depression. When the brain’s clock has stopped, the cellular power plants have shut down, inflammation is spreading, and the gut’s happiness factory has gone offline, demanding that someone “think positively” is not support, it is cruelty disguised as encouragement.
What you need is not self-blame, but a precise system-level restoration that repairs the biological machinery that has malfunctioned.
Yes, lifestyle habits such as morning sunlight, consistent sleep, hydration, and warm showers are helpful, but once the internal battery is completely depleted, it becomes nearly impossible to recharge through natural methods alone. At that point, scientific interventions are not optional; they are essential.
Healing begins when we stop moralizing depression and start treating it as the biological condition it truly is.
Stop blaming your mind, restore your biology. Discover science-based treatments to reboot your brain, gut, and energy systems, start today.
References
- Lyall LM, et al. Causal dynamics of sleep, circadian rhythm, and mood symptoms. eBioMedicine. 2024.
- Jiang M, et al. Mitochondria in depression: dysfunction of energy metabolism. CNS Neuroscience & Therapeutics. 2024.
- Ma K, et al. Microbiome-gut-brain axis as a novel hotspot in depression. Brain-X. 2024.
- Larrea D, et al. Mitochondrial Metabolism in Major Depressive Disorder. Journal of Clinical Medicine. 2024.












