Women’s Hormone Therapy

Menopause is the cessation of menstruation, a physiological change that typically occurs in women in their 50s as their biological rhythms shift. When menopause sets in, it signifies the end of a woman’s reproductive ability and a decline in the production of estrogen and progesterone—two key female hormones secreted by the uterus. This hormonal decline leads to various physical changes, with symptoms varying widely among individuals.
Common symptoms include mood swings, insomnia, night sweats, and vaginal dryness. Many menopausal women experience significant discomfort, but it is essential to recognize that these changes are a natural part of aging, similar to how acne occurs in teenagers due to hormonal fluctuations.
The issue arises when these natural changes are treated as a disease requiring medical intervention.
The History of Hormone Therapy and Controversies
In 1942, the U.S. FDA approved Premarin, a hormone replacement therapy (HRT) developed by Wyeth-Ayerst Pharmaceuticals to alleviate menopausal symptoms. Since then, numerous drugs and topical treatments have been introduced worldwide and prescribed to menopausal women. However, this practice has not been without controversy, particularly regarding whether menopause should be classified as a medical condition.
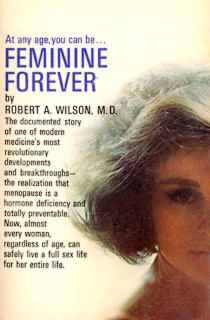
In 1966, New York-based gynecologist Robert Wilson published a book titled Feminine Forever, arguing that menopause should be regarded as a disease. He claimed that many physicians failed to acknowledge the severity of menopause, even though it could cause functional impairment and suffering.
Wilson’s book framed menopausal women as having “lost their femininity” and described their bodies as deteriorating. He argued that estrogen was essential for maintaining youth and attractiveness, making women more appealing to men. He even suggested that hormone therapy could prevent issues such as alcoholism, nicotine addiction, divorce, and family conflicts.
At the time, such male-centric views were widely accepted without much opposition. His claims, despite lacking scientific evidence, gained public trust, and media endorsements fueled the perception that menopause was a medical condition requiring treatment. As a result, Premarin sales skyrocketed, making it one of the three most prescribed medications in the U.S. by 1975.
However, concerns emerged when, later in 1975, the FDA reported that estrogen-based hormone therapy was linked to an increased risk of endometrial cancer, with 7.6% of users affected. This risk continued to rise over time.
Five years later, researchers at Boston University Medical Center conducted a study on 15,000 American women who had taken estrogen therapy between 1971 and 1975, analyzing its impact on endometrial cancer. (https://pubmed.ncbi.nlm.nih.gov/39522613/)
Types of Hormone Therapy and Risks
Menopausal hormone therapy primarily consists of:
- Estrogen-only hormone replacement therapy (HRT): Typically prescribed for women who have undergone a hysterectomy (uterus removal).
- Combination therapy (estrogen + progestin/progesterone): Used for women who still have their uterus.
Estrogen-only therapy can lead to endometrial hyperplasia, a condition where the uterine lining thickens excessively, increasing the risk of endometrial cancer.
Hormone replacement therapy is available in various forms, including:
- Oral tablets (systemic therapy)
- Transdermal patches, creams, gels, sprays, or vaginal rings
- Low-dose estrogen creams, suppositories, or rings (These primarily act on vaginal tissue with minimal absorption into the bloodstream.)
Health Risks Associated with Hormone Therapy
According to the Women’s Health Initiative (WHI)—a U.S. National Heart, Lung, and Blood Institute (NHLBI)-funded national health research program (https://www.whi.org/):
A study published on the National Institutes of Health (NIH) website titled Long-Term Risks of Combined Hormone Therapy Outweigh Benefits for Postmenopausal Women revealed that hormone therapy increases the risk of cardiovascular disease and breast cancer.
- Cardiovascular Disease: The risk decreases after stopping hormone therapy.
- Breast Cancer: Unlike cardiovascular disease, the increased risk persists even after discontinuing hormone therapy.
The study found that women who stopped combined hormone therapy (estrogen + progestin) were 27% more likely to develop breast cancer compared to non-users. Over a three-year period, 79 women in the treatment group were diagnosed with breast cancer. The lingering effects of hormone therapy indicate that regular breast exams and mammograms remain critical even after stopping treatment.
“The hormones’ effects on breast cancer appear to linger. These findings reinforce the importance of women getting regular breast exams and mammograms, even after they stop hormone therapy.” — Dr. Leslie Ford, National Cancer Institute (NCI), NIH
In addition to breast cancer, hormone therapy was found to increase the overall risk of other cancers by 24%.
The Long-Term Health Risks of Hormone Therapy
Prolonged use of combined hormone therapy is associated with increased cancer risks that persist even after stopping treatment. These findings confirm that the long-term health risks of menopausal hormone therapy outweigh its benefits.
For women undergoing hormone therapy, regular health screenings for breast and other cancers are strongly recommended to monitor potential risks.